The application of forward psychiatry among Malaysian soldiers on battlefield: Case Series
1Department of Psychiatry, Tuanku Mizan Armed Forces Hospital, Jalan 4/27a, Wangsa Maju, 53300, Kuala Lumpur, Malaysia
2Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kem Perdana Sungai Besi, 57000 Kuala Lumpur, Malaysia
*Corresponding Author:
Muhammad Farhan Nordin, Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kem Perdana Sungai Besi, 57000 Kuala Lumpur,
Malaysia,
Email: farhan@upnm.edu.my
Received: 25-Jul-2022, Manuscript No. AJOPY-22-71944;
Editor assigned: 26-Jul-2022, Pre QC No. AJOPY-22-71944 (PQ);
Reviewed: 12-Aug-2022, QC No. AJOPY-22-71944;
Revised: 22-Aug-2022, Manuscript No. AJOPY-22-71944 (R);
Published:
29-Aug-2022, DOI: 10.54615/22317805.47272
Abstract
Introduction: The forward psychiatry practice in the combat field has proven effective in reducing the attrition rates due to combat and operational stress of the service members. The concept has evolved over the years with the same objective to conserve the fighting troops' strength and minimize the incident rates of post-traumatic stress disorder among the soldiers. The Combat and Operational Stress Reaction (COSR) team has been deployed to the conflict zone and applied the forward psychiatry principles to the troops on the battlefield. Case Series: Here, we presented 3 case series of service members that were attended by the COSR team during their deployment on the frontline. First, a serviceman presented with late recognition of acute stress symptoms following active combat duty with poor support from his unit. Second, a combat engineer presented with anxiety and somatic symptoms after combat duty; third, a combat radio operator with early detection of acute stress symptoms by his unit commander. Results: In the first case, the patient's psychological condition deteriorated, requiring frequent sedation and transfer to a military tertiary hospital. In the second and third cases, both patients improved and returned to their duties with individualized psychotherapy and relaxation techniques. Conclusion: Early detection of the symptoms and intervention based on the principles of forward psychiatry in active combat zone facilitate service members' return to function and reduce complications and morbidity to their psychological health. ASEAN Journal of Psychiatry Vol. 23(8) August, 2022; 1-11.
Keywords
Forward Psychiatry, Combat Stress, Combat and Operational Stress, Battlefield, Acute Stress Reaction
Introduction
Combat and operational stress reaction or acute stress reaction is a syndrome with various symptoms, including changes in soldier behaviour, emotional and physiological responses, avoidance, and deterioration in personal and military functioning during combat or military operations [1]. Although exact figures of the incident rate of combat stress are unknown, it is estimated that around 51.7% of previously deployed American service members have witnessed their team members develop acute stress reactions [2]. While acute stress reactions typically resolve quickly in the span of hours to three days, they might be hazardous and life-threatening to their team members and themselves due to the nature of their occupation and environment [3]. Forward psychiatry services have been utilized to reduce the impact of combat and operational stress on service members [4.5].
Malaysia is not excluded from the war, ranging from high-intensity war, such as in World War II, to intermittent and guerrilla-type of war, such as in Communist Insurgency, Lahad Datu Standoff, and UN peacekeeping missions. The Combat Stress Operational Team (COSR) consisted of army psychiatrists and paramedics deployed to mitigate the psychological impact of the frontline soldiers in the combat zone. The illustrated case series showed the application of forward psychiatry by the COSR team to the frontline soldiers in the conflict area.
Case 1
A 31-years-old corporal from the infantry battalion was transferred to a forward hospital from a civilian tertiary hospital. He was allegedly shot in the back by the militants before the presentation to the forward hospital. He was a section commander, and a group of militants had ambushed them, and he was protecting his comrade from the shot of a militant during that time. Fortunately, he wore an armored vest and only sustained soft tissue injury.
He was admitted to the civilian hospital for four days for treatment. During the admission, he had insomnia, hyper vigilant, irritability, and frequent verbal arguments with the treating doctors and nurses. He kept a knife below his pillow and pulled the bed curtain to cover his bed daily. He felt insecure being admitted to a civilian hospital as he felt that the militants would find and kill him in the hospital. There was no visitor or call from his unit to inquire about his condition throughout the admissions.
After discussions between the military medical officer and medical doctors from the tertiary civilian hospital, he was transferred to the forward hospital for further intervention. During his admission to the forward hospital, he still had sleep difficulties, was easily irritable, and had hyperarousal symptoms, especially towards loud sounds. His unit did not pay a visit to him, which led him to believe that his unit neglected him, and he expressed his frustration to the medical officer-in-charge. He also conveyed his intention to shoot his Commanding Officer (CO) when discharged to his unit. He was restless and wandering around the ward at the forward hospital and kept repeating his homicidal intention to kill his superiors; thus, the firearms and sharp objects were withheld from him, and he has been
prescribed T Midazolam 10mg ON. He was immediately transferred to the tertiary military hospital in Kuala Lumpur for further intervention. He was later diagnosed with Post Traumatic Stress Disorder (PTSD), started on Selective Serotonin Receptor Inhibitors (SSRI), and was medically discharged from the military.
Case 2
A 23- years-old combat engineer was first referred to the forward hospital with a chief complaint of left-hand pain and weakness for three days. He was admitted to the forward hospital for pain management and close observation. During the observation, the medical team noticed that the weakness and pain only occur when paramedics or doctors are present. There was no impairment in his daily activity living, and he could move the affected hand well. On day three of admission, he was referred to the combat stress reaction team. Upon further history, he had served in the military as a plumber for three years.
During the standoff, he was tasked to inspect any unexploded missiles or bombs and to search and destroy any booby traps and Improvised Explosive Devices (IEDs). He felt anxious and not confident about performing his task as this he felt incompetent to do so and worried someone might get killed if he missed the explosives. He was taught on few relaxation techniques by the deployed occupational therapist, such as deep breathing exercises and progressive muscle relaxation. The occupational therapist gave him supportive psychotherapy and group therapy for a few sessions. His squad leader was kept updated about his conditions during the regular visit to the COSR unit, and he was discharged well to his unit. He was given light duty, and with supervised gradual exposure at his unit, he assumed his regular combat duty.
Case 3
A 28-years old radio operator was referred by his Officer in Command (OC) after he was noted to have delayed response during and after the contact with the enemy militants during combat patrol. He presented with a blank stare and needed a prompt to answer the question. He stated that he was unprepared for real-life contact with the enemy and was scared during that time. His thoughts were blank and frozen, and he felt clueless. Upon assessment by the COSR team, he was given daily supportive psychotherapy and was treated at his company aid post. He was given off duty for a few days and rested at his unit under the supervision of his OC and Company Sergeant Major. After two days of rest, he returned to his unit and resumed his usual task.
Discussion
The principles of forward psychiatry were first applied by the French army and later devised by Thomas Salmon by introducing the PIE approach (Proximity to battle, immediacy, expectation of recovery) [6]. The principle was to detect and treat the afflicted soldiers near the combat zone, replenishing their physiological needs with minimal and straightforward psychiatric intervention.
The aim was to make the soldiers return to the warzone swiftly. The effectiveness of the practice of forward psychiatry in various wars since World War I showed that more than 80% of the soldiers from the combat troops returned to active duty [7,8]. Since World War I, psychotherapy treatments in the combat zone were integrated into the forward psychiatry management, using combination, simplicity, and brevity methods [9]. The principle of forward psychiatry has been evolving from 'PIE' ( Proximity to battle, immediacy, expectation of recovery) to 'BICEPS' ( Brevity, immediacy, contact/centrality, expectancy, proximity, simplicity) [10].
Another method that can be administered, especially in the small unit, is iCOVER. United States Army adapted it from YaHaLOM, a peer-to-peer intervention for acute stress reactions developed by the Israeli Defence Force. iCOVER comprises six components: 1) Identify the soldier is having an acute stress reaction, 2) Connect with the affected soldier, 3) Offer Commitment, 4) Verify facts, 5) Establish the order of events, and 6) Request action from the soldier to reduce the sense of uselessness and prompt their engagement in purposeful actions [3,11]. The management of combat stress reactions in the frontline is mainly non-pharmacological. If medications were needed, they were administered as a chemical restraint when treating acute psychosis or agitation while waiting for evacuation. Social connectedness and close relationship with other service members on the frontline is critical in determining the detection and prognosis of combat stress reactions.
The radio operator in case 3 has a good prognosis due to multiple favorable factors such as early symptoms detection by his superiors and appropriate therapy at the company aid post, where he had full support from his comrades. In contrast, the corporal in Case 1 demonstrated a lack of proximity to his unit, resulting in subsequent support discontinuation from his squad. His psychological injury was not detected quickly enough, resulting in resentment and perceived abandonment by his unit, which led to his later progression to PTSD. According to a few studies, social connectedness can moderate the effects of PTSD [12,13]. Social connectedness also is a protective factor in suicidality among older male veterans [14] (Table 1).
Table 1: Factors leading to Combat and Operational Stress Reaction/ Acute Stress Reaction (20-22)
| Factors Leading to Combat and Operational Stress Reaction/ Acute Stress Reaction |
| Trauma |
| Exposure to trauma, dangers, and loss |
| Target of physical, psychological, or sexual abuse |
| Combat and Operation Conditions |
| Lengthy and frequent deployments |
| Repetitive or monotonous work |
| High workload – long hours and heavy demands |
| Equipment malfunction or shortage |
| Ambiguous missions and objectives of the deployment |
| Inconsistent rules of engagement |
| Training and mission discrepancy |
| Prolonged combat duty |
| High-intensity combat |
| Bombardment by the enemy force |
| Holding a defensive position |
| Organization and Leadership |
| Reserve unit |
| Lack of planning |
| Pessimistic rumors |
| Lack of trust in leadership |
| Avoidance of talking about personal feelings |
| Lack of support from leadership, unit, or others |
| Adverse career events - legal or administrative problems |
| Environment of Operation |
| Challenging operation areas - isolation, harsh landscape, and extreme climate |
| Operation in countries with different cultures |
| Working with an army of different cultures |
| Personal and Physical Adversity |
| Loneliness |
| Illness and injury |
| Sleep deprivation |
| High physical demands |
| Inadequate food, water, and sanitation supply |
| Loss of belief in the legitimacy of the mission |
| Previous history of psychiatric disorders |
| History of substance use |
| Work-Life Conflict |
| Separation from family and friends |
| Financial difficulty |
| Stressful events in the family – marital problems, illness, or death |
| Career priorities vs. domestic responsibilities |
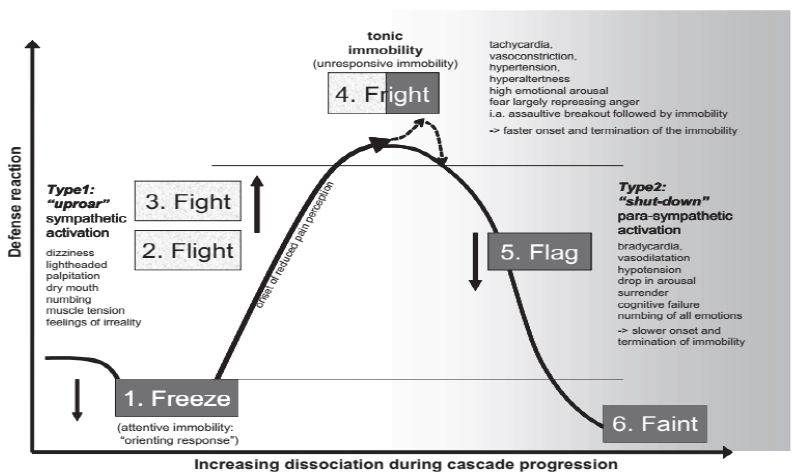
The widely known theory of the ‘fight or flight’ response in the face of threat and trauma has been expanded in the defense cascade model, which is the ‘freeze – flight – fight – fright – flag – faint’ response, as illustrated in Figure 1 [15,16]. In Case 3, the radio operator may have been in the shutdown phase characterized by a blank stare, thought block, and immobility. Although not all patients exposed to trauma are presented with dissociation, this cascade hypothesized why some patients might present with psychosomatic symptoms during or after exposure to stressful conditions on the battlefield [17]. In Case 2, the combat engineer presented with somatic complaints, pain, and weakness of the limbs after being tasked to search and destroy bombs and Improvised Explosive Devices (IEDs). Luckily, with early detection and referral to a multi-disciplinary COSR team, the patient recovered and returned to his duty. It has been documented that civilian and military personnel who suffer from acute stress disorder and PTSD may present with somatic complaints. A systematic review by Afari et al. has shown that a person exposed to trauma is 2.7 times more likely to have functional somatic syndrome. Another real-life report from the 2020 Nagorno-Karabakh War found an inverse correlation between physical injury and psychological injury post-exposure to trauma; a person who suffered mild to no physical injury is more expressive about psychological injury and vice versa.
Early detection of somatic and psychological symptoms (Table 2) of combat and operational stress among military personnel on the battlefield is of utmost importance. As illustrated in Case 2 and Case 3, both recovered and were able to return to their duty. In contrast, late detection and intervention of combat stress may lead to further deterioration and inability to perform their assigned duty, as illustrated in Case 1. In a study by Jones et al., 75% of frontline mental health casualties in Afghanistan returned to combat duty after receiving assessment or therapy by deployed mental health practitioners [4]. As described earlier, few techniques have been proposed for the early intervention of combat and operational reactions, including early and appropriate therapy by the frontline mental health practitioners or iCOVER as a peer-to-peer intervention at the unit level.
Table 2: Signs and symptoms of combat and operation stress reaction/ acute stress reaction (15,23)
| Clinical profile |
Arousal phase |
Shutdown Phase |
| Physiological changes |
|
|
| Pulse rate |
Increased |
Reduced |
| Blood pressure |
Raised |
Reduced |
| Breathing pattern |
Fast and deep |
Slow and shallow, shortness of breath |
|
|
Drained, weak |
| Energy level |
Increased |
Reduced |
| Body temperature |
Raised |
Increased tears, smaller pupils |
| Eyes signs |
Dry eyes, enlarged pupils |
Increased appetite and salivation |
| Appetite and digestion |
Decreased appetite, dry mouth |
Incontinence |
|
|
Sleepiness |
| Urinary and bowel |
Reduced elimination |
|
| Sleep |
Difficulty falling or staying asleep; nightmare |
Shivering, limp muscle |
|
Sweating, goosebumps, muscle jerks, twitches |
|
| Skins and muscles |
Lightheadedness, dizziness |
Nausea, vomiting |
| Neurological symptoms |
|
|
| Behavioral and emotional symptoms |
|
|
| Activity |
|
|
|
Agitation, restlessness, recklessness |
Frozen, paralyzed, collapsed |
| Social |
Over-excitement, arguing, fighting within the unit |
|
|
|
Social withdrawal, unresponsiveness, disconnected from the unit |
|
Temper outbursts, euphoria, panic attacks, crying, fleeing, mood swings |
Extreme fear, hopelessness, numbness, emotionless |
| Emotion |
Hyperarousal, exaggerated startle response, over-focussed on the threat, feeling of unreality |
|
|
|
Non-responsive, lack of awareness, unable to focus or respond to the immediate threat, loss of startle response and other reflexes, loss of sense of self and surrounding |
| Awareness |
|
|
| Cognitive symptoms |
Rapid thinking, confusion, memory problems, poor judgment |
Sluggish, disorientation, thought block, memory loss, Indecisiveness |
| Speech pattern |
Loud, rapid, or stuttering |
Soft, mumbling, or mute |
| Sensorimotor symptoms |
Exaggerated sight, hearing, or feeling |
Inability to see, hear or feel |
| Tingling sensations |
|
| Reduced pain |
Numbness |
|
Failure to feel pain |
*Some of the signs and symptoms associated with COSR/ASR are associated with other life-threatening conditions which need to be ruled out first through thorough assessments and investigations by licensed healthcare providers
Conclusion
Combat and operational stress reactions can present heterogeneous behaviours, and cognitive and affective manifestations, leading to impairment of function. Mental health awareness and promoting psychological resilience in the unit are imperative for combat effectiveness. It requires a concerted effort from multiple parties, including the individual, unit leader, and deployed mental health practitioners, to prevent or mitigate the negative setbacks in the military operation and eventually conserve the troops' fighting strength. We also hope that the lessons learned from these case series may guide the future development of stress management programs in military and other non-military stressful situations.
References
- Gindi S, Galili G, Volovic-Shushan S, Adir-Pavis S. Integrating occupational therapy in treating combat stress reaction within a military unit: An intervention model. Work. 2016; 55: 737–745.
[Crossref] [Google Scholar] [Indexed]
- Adler AB, Svetlitzky V, Gutierrez IA. Post-traumatic stress disorder risk and witnessing team members in acute psychological stress during combat. BJPsych Open. 2020; 6: 1–7.
[Crossref] [Google Scholar] [Indexed]
- Svetlitzky V, Farchi M, Ben Yehuda A, Adler AB. YaHaLOM: A Rapid Intervention for Acute Stress Reactions in High-Risk Occupations. Mil Behav Heal 2020; 8: 232–242.
[Crossref] [Google Scholar] [Indexed]
- Jones N, Fear NT, Wessely S, Thandi G, Greenberg N. Forward psychiatry – early intervention for mental health problems among UK armed forces in Afghanistan. Eur. Psychiatry. 2017; 39: 66–72.
[Crossref] [Google Scholar] [Indexed]
- Richter KE, Jones DE, Oliver DM. Making mental health aerovac decisions in Afghanistan: A field report. Mil Med 2012; 177: 507–510.
[Crossref] [Google Scholar] [Indexed]
- Jones E, Wessely S. 'Forward psychiatry' in the military: Its origins and effectiveness. Trauma. Stress. 2003; 16: 411–419.
[Crossref] [Google Scholar] [Indexed]
- Jones E, Wessely S. Psychiatric battle casualties: An intra- and interwar comparison. Br J Psychiatry 2001; 178: 242–247.
[Crossref] [Google Scholar] [Indexed]
- Helmus TC, Glenn RW. Steeling the Mind: Combat Stress Reactions and Their Implications for Urban Warfare. RAND Corporation 2005.
- Glass AJ. Psychotherapy in the Combat Zone. Am J Psychiatry 1954 ; 110(10) : 725–731.
[Crossref] [Google Scholar]
- Smith-Forbes E, Najera C, Hawkins D. Combat operational stress control in Iraq and Afghanistan: Army occupational therapy. Mil Med 2015; 179: 279–284.
[Crossref] [Google Scholar]
- Adler AB, Adler A, Start A, Milham L, Yvonne Allard, Dawn Riddle, Lisa Townsend, Vlad Svetlitzky et al., Rapid Response to Acute Stress Reaction: Pilot Test of iCOVER Training for Military Units. Psychol. Trauma Theory, Res. Pract. Policy 2019; 12: 431–435.
[Crossref] [Google Scholar]
- Kintzle S, Barr N, Corletto G, Castro CA. PTSD in US veterans: The role of social connectedness, combat experience and discharge. Healthc 2018 ; 6 :4–10.
[Crossref] [Google Scholar] [Indexed]
- Schwartz E, Shrira A. Social Connectedness Moderates the Relationship Between Warfare Exposure, PTSD Symptoms, and Health Among Older Adults. Psychiatry New York 2019; 82: 158–172.
[Crossref] [Google Scholar] [Indexed]
- Fanning JR, Pietrzak RH. Suicidality among older male veterans in the United States: Results from the National Health and Resilience in Veterans Study. J Psychiatr Res 2013 ; 47 : 1766–1775.
[Crossref] [Google Scholar] [Indexed]
- Afari N, Sandra M, Ahumada LJ, Wright S, Veronica Reis JG, et al., Psychological trauma and functional somatic syndromes: A systematic review and meta-analysis. Psychosom Med 2014; 76 : 2–11.
[Crossref] [Google Scholar] [Indexed]
- Hovhannisyan HR, Tarjumanyan SV, Barseghyan AA. The Psychosomatic Relationship Between Combat Stress and Injuries (Monitoring Results Report). Mod Psychol 2021; 4: 199–204.
[Crossref] [Google Scholar]
- Schauer M, Elbert T. Dissociation following traumatic stress etiology and treatment. Zeitschrift fuer Psychologie. Journal of Psychology. 2010; 218(2): 109–27.
[Crossref], [Google Scholar]