Abstract
Objectives: Soldiers can manifest a wide range of psychological symptoms that varies from anxiety, depression to somatic symptoms in combative and non-combative situations. This paper aims to discuss the issue related to the challenges of establishing the diagnosis of a soldier in a stressful non-battlefield condition. Methods: We herein report a young soldier with no underlying medical condition who presented with initial abnormal behaviour associated with progressive mutism for two years. Physical examination was unremarkable. Relevant blood investigations and Magnetic Resonance Imaging (MRI) brain revealed no abnormalities. He was initially treated as brief psychotic disorder and was revised into Schizophrenia based on Diagnostic and Statistical Manuals of Mental Disorders (DSM-5) and was started on antipsychotics. However, he showed no improvement after two years on treatment. He was on the verge of being discharged from the service due to medical reasons. Therefore, he was readmitted to the ward for evaluation of the diagnosis while all of his medications were withheld. Different psychological approaches including supportive therapy and occupational therapy were employed. Results: Following series of individual supportive therapy sessions, we uncovered the unconscious psychological conflicts within him. He gradually started to communicate verbally and his psychosocial functions began to improve. Upon discharged, the soldier was diagnosed as Functional Neurological Symptom Disorder. Conclusion: A thorough and careful evaluation was crucial in assessing patients with progressive mutism to ensure a correct diagnosis was made. In a patient who failed to improve after optimum treatments were given, a different approach may be utilized to explore the possible factors that hindered the patient recovery.
Keywords
Mute, Soldier, Functional Neurological Symptom Disorder, Conversion, Disorder
Introduction
Selective mutism is defined as unwillingness or inability to speak and results in marked paucity or absence of verbal output that could be due to various conditions, both organic or functional [1].
In children, mutism is associated with a range of emotional or psychiatric disorders while mutism in adults is known to be associated with hysteria, depression, schizophrenia or organic brain disorders [2]. Hence, making the correct diagnosis is very crucial to determine the management of the patient.
This case report illustrates a soldier presented with progressive mutism for two years and the challenges faced during the management.
Case Report
Mr. R is a 25-year-old male soldier who had just completed his military training and was doing his five-month induction course at the army academy. However, during the final month of the course, he presented with a brief, sudden onset of abnormal behaviour described as performing Malay martial art and Yoga inappropriately associated with refusal to talk for three consecutive days 9 (Table 1). He was admitted to a military hospital for six days before being transferred to a military hospital nearby his home upon the family request.
Table 1: Psychological causes of mutism
| Schizophrenia |
Catatonic paranoid
disorganized |
| Affective disorder |
Major depressive disorder
Bipolar disorder |
| Other psychotic disorders |
Schizophreniform disorder
Schizoaffective disorder brief psychotic disorder
Atypical psychosis |
| Somatic symptoms and related disorders |
Functional neurological symptoms disorder
Factitious disorder |
| Dissociative Disorders |
Dissociative identity disorder
Dissociative amnesia |
During admission, his mental state examination revealed a thin built young man with poor rapport and minimal eye contact. He was mute and only responded occasionally to questions via writing, where the answers were relevant but minimal amount. No hallucinatory or abnormal behaviour being observed. Depressive and manic symptoms were not elicited. He was alert and conscious. His vital signs were within normal limit. Neurological examination including cranial nerves examination was normal. There was no bruise or any evidence of external injury being documented. Relevant blood investigations, urine for drug screening and Magnetic Resonance Imaging (MRI) brain showed no significant findings. Limited collaborative history from the colleagues and family members were suggestive of stress-related issues.
Pre-morbidly, Mr R was described as an obedient son who is keen to please his parents. His academic performance was average and had completed his diploma in automotive engineering. He worked at various places before his father convinced him to become a soldier in order to have a stable job and income. Mr R has a maternal aunt who was receiving treatment for psychotic disorder.
Mr R was initially diagnosed with brief psychotic disorder based on Diagnostic and Statistical Manual of Mental Disorder (DSM-5) [3]. Within two weeks of admission, his condition worsens whereby he appeared perplexed, mute and there was slowness in his movement and responses. He was no longer communicating via writing but still able to follow instruction and communicate via making some gestures. He needs to be prompted for self-hygiene and Activities of Daily Living (ADL).
Treatment was a challenge in this patient. Initially olanzapine 10 mg, fluoxetine 40 mg and clonazepam 2 mg daily were prescribed for five months. Due to his poor response, the diagnosis was revised to schizophrenia and all medications were tapered off and replaced with aripiprazole 15 mg daily and zolpidem 10 mg at night. He was compliant to the medications. Unfortunately, over a span of almost two years since the onset, he showed minimal improvement (Figure 1). Although his parents were very concerned that these problems could signal a serious medical illness, Mr. R. neither appeared alarmed nor anxious. He was on the verge of being discharged from the military service due to medical reasons. Therefore, he was admitted to the ward for final assessment and reevaluation of diagnosis and treatment.
In the ward, his behavior was observed, and all his medications were withheld. He was referred to the occupational therapist for individual social skills training, cognitive training, anger management techniques, and positive coping and relaxation techniques. While in the ward, he was accompanied by another soldier from his unit and received regular visits from the superior. He was encouraged to wear the uniform as part of reintegration into the working environment. He was cooperative even though he remained mute and communicating only by limited gestures and writing.
Slowly, he was able to gain trust with the treating psychiatrist and the therapeutic alliance was formed within 2 weeks of admission. Following series of individual supportive therapy, he started to speak in whispering voice and began to communicate. We were able to unravel the unconscious psychological conflict in the patient. Mr. R alleged that he was physically and mentally bullied by his colleagues. He was threatened with more severe consequences if he reported the incident to the superior. He was feeling ambivalent, scared and entrapped in the situation. As a result, he had difficulty to trust the people in the military uniform. Mr. R was given appropriate reassurance and encouragement from the treating team. He participated actively during the sessions with occupational therapist. He was discharged after showing a significant improvement within one month of admission to the ward with a final diagnosis of Functional Neurological Symptoms Disorder (FNSD).
Discussion
The heterogenicity of the psychological reactions in the unwounded soldier makes the diagnosis complicated especially when the soldier is mute, unresponsive, or aggressive. Mr R’s predominant presenting symptoms were progressive mutism and psychomotor slowness. Patient with mutism is often closely associated with catatonia [4]. The clinical presentation of catatonia can be incomprehensible, as the psychomotor disturbance may range from marked unresponsiveness to marked agitation. Even in the same individual, the symptoms can fluctuate with decreased and excessive motor activities [5]. The conflicting clinical presentation posed greater challenges for the diagnosis as seen in this patient.
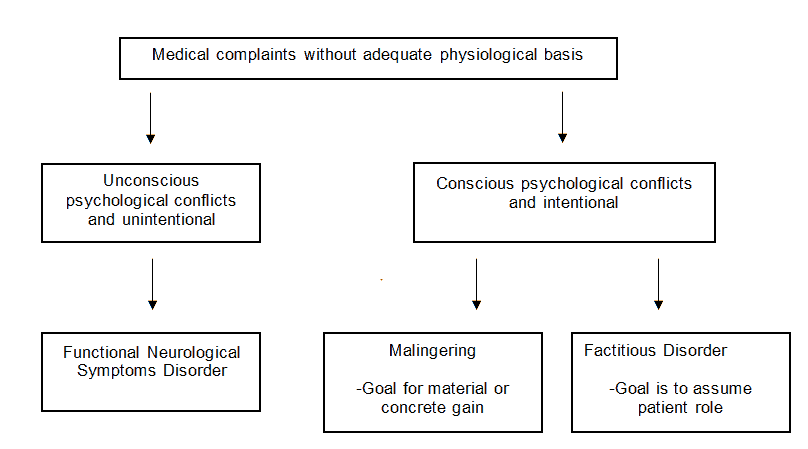
While a major part of psychiatric assessment is usually done through verbal interview, this technique is not applicable in the case of mutism. The treating team faced with dilemma of needing to rely on the observation and non-verbal assessments supported by the collaborative history as the biological and imaging investigations were unremarkable. He received treatment for psychotic disorder but with minimal improvement seen for almost two years. The revision of diagnosis to FNSD (need to spell out first time used in the paper) or previously known as conversion disorder requires a high level of suspicion especially in atypical presentation like Mr. R. The more common neurological presentation of FNSD includes motor weakness, non-epileptic seizure or abnormal sensation [6]. The essence here is to look at overall clinical picture integrating abnormal thought, feeling and behaviour rather than focusing on the specific symptom itself. In this case, there were ‘LaBelle indifference’ and incongruity between the clinical presentation and absence of organic pathology that provided cues to the treating psychiatrists about the possibility of FNSD [7]. In FNSD, the patient usually has underlying unconscious psychological conflicts that presented with neurological symptoms such as paralysis, blindness or other sensory deficits which was unexplained by any known medical condition. It is also important to note that the neurological symptoms were not feigned by the patient.
From psychoanalytical point of view, this case posed more challenges as he is in a military service. As a soldier, he is trained to have courage, honour, integrity, patriotism, self-sacrifice and loyalty. Obedience is a very important aspect in military training for fast and efficient military action without hesitation [8]. Mr R. has a significant unconscious psychological conflict when he was bullied by senior colleagues whom he needs to hide his feeling but to show his respect to the seniors. This situation produced a repression of unconscious intrapsychic conflict which manifested as mutism.
The neurological symptom in conversion disorder usually has a ‘symbolic’ meaning to the underlying psychological conflicts. In this situation, mutism may symbolise that he is a loyal soldier who is able to uphold the secret of him being bullied. It also enabled him to evade questions regarding his absence from the duty while at the same time provide a ‘safe’ escape route from remaining in the perceived threatening situation. These psychodynamic understanding about life events and escape in FNSD had helped the treating psychiatrists to provide the necessary psychosocial supports and facilitated the recovery process [9]. The supportive stance that was utilized by the treating team in order to establish a strong therapeutic alliance in this case was proven to be a success when these hidden conflicts were disclosed.
The role of Occupational Therapy (OT) in managing a distress soldier was crucial in this case. Individualized OT sessions have been proven to improve the Return-To-Duty (RTD) rates among soldiers who suffered combat and operational stress in the past [10-12]. Similar approach was also found to be useful in this non-battlefield situation.
The reconditioning program that was initiated in the ward also played a significant role in this patient’s recovery. In the past, the reconditioning program is initiated for soldiers who were recovering from physical injuries to promote physical fitness [13]. Similar approach can be used for rehabilitation process of soldiers with psychological problems. Another purpose of this program was to promote the unit cohesion which has been proven to be an important mitigating factor that buffers the soldiers from various mental health issues in combative situations. To date, Mr. R has shown a tremendous progress in his psychosocial and had started working at his unit as a technician. He remained in the military service and received remarkable and encouraging support from his superiors as well as his family.
Conclusion
In summary, patients with functional neurological disorders/conversion disorder usually present with a diagnostic challenge due to their complex presentation. In military setting, collaborative efforts in between the psychiatric team, occupational therapist, military unit and family members should be utilized to maximize the chance of recovery for a distress soldier who suffers from functional neurological symptoms disorder.
Acknowledgement
The authors would like to acknowledge the contribution of Prof. Dr. Yasmin Anum Binti Mohd Yusof in proofreading the manuscript and Kol (Dr) Nordiana Binti Dollah for providing invaluable support throughout the writing process.
References
- Aggarwal A, Sharma DD, Kumar R, Ramesh Kumar. Mutism as the presenting symptom: three case reports and selective review of literature. Indian Journal of Psychological Medicine. 2010; 32(1): 61-64.
- Casey P, Kelly B. Fish’s clinical psychopathology. In: fish's clinical psychopathology: signs and symptoms in psychiatry. Cambridge University Press. 2019.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th edition). Arlington, VA: Author 2019.
- Dutt, A, Grover S, Chakrabarti S, Avasthi A, Kumar S. Phenomenology and treatment of catatonia: A descriptive study from north India. Indian Journal of Psychiatry. 2011; 53(1): 36–40.
- Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology. World Journal of Psychiatry. 2016; 6(4): 391–398.
- Gilmour GS, Nielsen G, Teodoro T, Yogarajah M, Coebergh JA, et al., Management of functional neurological disorder. Journal of Neurology. 2020; 267(7): 2164–2172.
- Gokarakonda SB, Kumar N. La Belle Indifférence. In: Stat Pearls. Treasure Island (FL): Stat Pearls Publishing. 2021.
- Wolfendale J. Obedience in the Military. In Torture and the Military Profession. Palgrave Macmillan, London. 2007.
- Nicholson TR, Aybek S, Craig T, Harris T, Wojcik W, et al., Life Events and Escape in Conversion Disorder. Psychological Medicine. 2016; 46(12): 2617-2626.
- Montz R, Gonzales F Jr, Bash DS, Carney A, Bramlett D. Occupational therapy role on the battlefield: an overview of combat and operational stress and upper extremity rehabilitation. Journal of Hand Theraphy. 2008; 21(2): 130–135.
- Smith-Forbes E, Najera C, Hawkins D. Combat Operational Stress Control in Iraq and Afghanistan: Army occupational therapy. Military Medicine. 2014; 179(3): 279-284.
- Smith-Forbes EV, Quick CD, Brown KM. Roles of Occupational Therapists in Theater, Past and Present. US Army Medical Department Journal. 2016; 16: 66-70.
- Barton WE. The Reconditioning and rehabilitating program in army hospitals. American Journal of Psychiatry. 1945: 101(5): 608-613.
- Campbell-Sills L, Flynn PJ, Choi KW, Ng THH, Aliaga PA, et al. Unit cohesion during deployment and post-deployment mental health: Is cohesion an individual-or unit-level buffer for combat-exposed soldiers. Psychological Medicine. 2020; 1-11.