MASSIVE OSSIFICATION OF THE RIGHT PATELLA AND SURROUNDING SOFT TISSUE CAUSED BY OPEN TRAUMA AND ITS TREATMENT: CASE REPORT
1Department of Orthopaedics, The First Affiliated Hospital of Shenzhen University, Guangdong, China
2Department of Orthopaedics, Jinan University, Guangdong, China
3Department of Medicine, Shenzhen University School of Medicine, Guangdong, China
*Corresponding Author:
Aobulikasimu Aikebaier, Department of Orthopaedics, The First Affiliated Hospital of Shenzhen University, Guangdong,
China,
Email: akbaramqi@yeah.net
Received: 01-Sep-2022, Manuscript No. AJOPY-22-73497;
Editor assigned: 05-Sep-2022, Pre QC No. AJOPY-22-73497 (PQ);
Reviewed: 20-Sep-2022, QC No. AJOPY-22-73497;
Revised: 27-Sep-2022, Manuscript No. AJOPY-22-73497(R);
Published:
04-Oct-2022, DOI: 10.54615/2231-7805.S2.003
Abstract
Introduction: Heterotopic Ossification (HO) refers to the presence of new bone in soft tissue. It occurs mostly around large joints, such as the hip and elbow, but it is rare in the patella and patellar ligaments. In this article, we describe a rare case of Massive ossification of the right patella and surrounding soft tissues, mainly caused by open trauma, and describe its treatment. Low-grade inflammation and hyper activation of the sympathetic nervous system during psychological stress are also physiological changes detrimental to bone health.
Case presentation: The 41-year-old male patient had a history of repeated pain and limited mobility of the right knee joint beginning 5 years previously and severe limitation of mobility of the right knee joint of 1 year. The auxiliary examination on admission were as follows: X-ray examination results showed degenerative changes in the right knee joint, an unequal length of lower limbs, and a tilted pelvis. CT examination revealed extensive tendon calcification and joint degeneration in the right knee. MRI of the right knee revealed degenerative changes of the right knee, which was considered to be caused by extensive tendon ossification of the right knee, grade 2-3 damage to the lateral meniscus in the right knee, an obvious medial posterior horn, and a small amount of fluid accumulation in the cavity and joint capsule of the right knee. The patient underwent a total joint replacement operation under general anesthesia and experienced immediate pain relief and full restoration of knee range of motion.
Conclusion: This is the first report of extensive ossification of the patella and surrounding tissues resulting in knee pain and limited knee mobility. Based on the literature review, this case describes the difference between patella ossification and calcification and related factors leading to patella ossification. The case showed a good prognosis after surgical treatment. ASEAN Journal of Psychiatry, Vol. 23(S2) September, 2022; 1-8.
Keywords
Ectopic Ossification, Patellar Ligament, Ligament Ossification, Joint Surgery Sequelae
Abbreviations
HO: Heterotopic Ossification; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; VAS: Visual Analogue Score; BMP1: Bone Morphology Protein1; FOP: Fibrodysplasia Ossificans Progressiva; ACVR1: Activvin A Type 1 Receptor Gene; MSC: Mesenchymal Stem Cells
Background
Heterotopic ossification is the new mature bone formation in normal non-osseous soft tissue. Heterotopic ossification is easily confused with metastatic calcification (as is common with hypercalcemia) and calcification with malnutrition (as is common in tumorous tissues) [1]. Trauma, surgery, burns, and nervous system damage can lead to heterotopic ossification [2-4] Trauma and surgical causes are reported to be most common in hip replacement or acetabular fractures, causing up to 90% of cases, after certain types of hip arthroplasty or acetabular fractures [5,6]. The next most common site of injury is the elbow [7]. When the burned area reaches 25% of the total surface area, HO occurs in up to 35% of cases. We here report for the first time a large area of ossification of the patella and surrounding soft tissue after repeated arthroscopy. The return to the normal functioning status of the patients suffering from HO is often retarded with different rates of psychological improvement. Patients who are susceptible to developing HO develop and evolve clinical features including psychiatric presentations with seizures.
Case Presentation
The 41-year-old male patient was admitted to the hospital with the chief complaint of right knee pain without an obvious cause for 5 years, as well as aggravation resulting in limited extension and flexion beginning more than 1 year previously. Five years before admittance, the patient developed right knee pain without obvious inducement, which was obvious during activity and relieved during rest. During the past year, the pain in the right knee joint became worse and flexion and extension were limited. Through MRI examination of the right knee, he was diagnosed with free body of the right knee, chronic synovitis, and underwent arthroscopic surgery. There was no significant relief of symptoms after arthroscopy. Physical examination on admission revealed that the right knee joint experienced pain and redness, and the local skin temperature of the right knee was higher than that of the opposite side. There were 3 scars 1 cm in front of the right knee (after knee arthroscopy), obvious tenderness of the patellar tendon, and tenderness in the front of the medial and lateral joint space, even when the mass was not touched. The patellar wear test was (-), the floating patellar test was (+), flexion was 40º, extension was -20º, and range of motion was 20º, the VAS score was 8. There was no obvious abnormality of the contralateral knee joint [8].
The auxiliary examination results are as follows
The X-ray examination results showed hyperosteogeny at the surface and edge of the right knee, a slight sharpening of the intercondylar protuberance, increased bone density of the right knee, bony fusion of the lower edge of the right patella and the proximal tibia, narrowing of the space of the right knee, and an unequal length of both lower limbs, with the right side being slightly shorter. CT examination results showed extensive bone hypertrophy and hyperplasia of all bone components of the right knee joint, extensive calcification of multiple ligaments-especially the patellar ligament, the bony fusion between the patella, and tibial tuberosity-bony fusion of the proximal tibiofibular bone, narrowing of joint space, and a small amount of fluid accumulation. MRI results showed right patellar ligament increases; mixed signals for adjacent soft tissue; fusion of the proximal tibia fibular bone; fused edges of bone hyperplasia; some effusion of the articular cavity; with the angle more obvious after the medial meniscus; anterior cruciate ligament enlargement without clear edges; and soft tissue swelling under the skin. One year previously, she underwent arthroscopic surgery in another hospital because of synovitis of the right knee joint and loose body.
Investigations
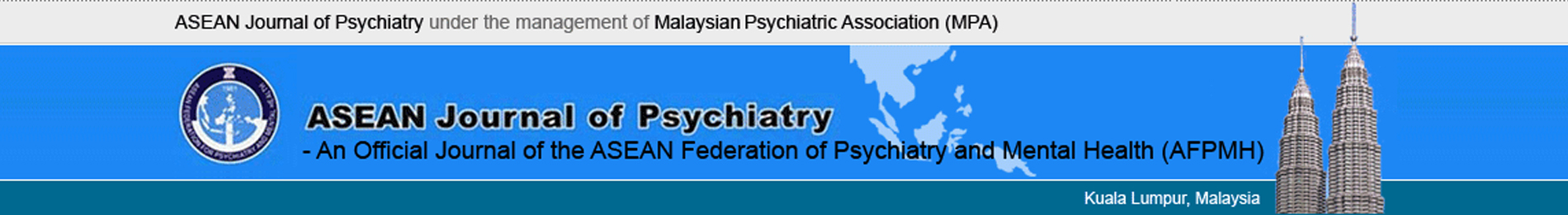
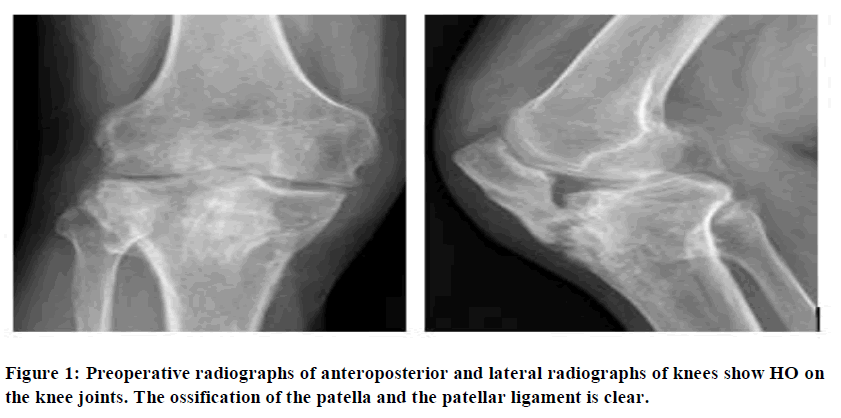
Systemic blood sampling was performed during the patient’s hospitalization. Anteroposteroidal radiographs of the right knee showed hyperosteogeny on the articular surface and the edge of the right knee and slight sharpening of the intercondylar carina. The right knee showed high bone density, the lower edge of the right patella was fused with the proximal tibia, and the space of the right knee had narrowed (Figure 1). Right knee CT examination results show that the right knee had bone hypertrophy, hyperplasia, and broad ligament calcification; most significantly that of the patellar ligament, between the patella and tibial tubercle. There was a small amount of effusion (Figure 2).
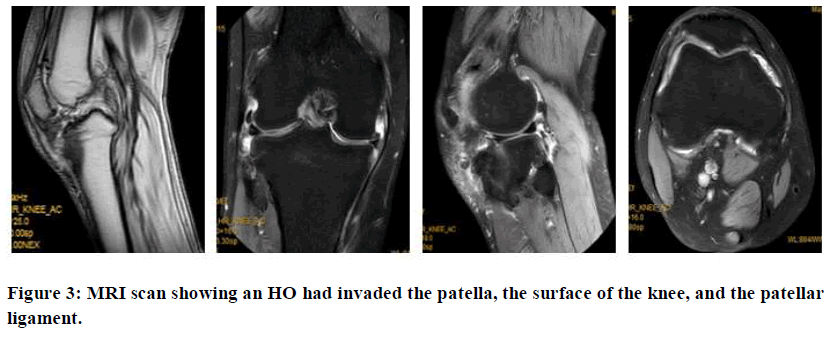
MRI examination results of the right knee showed readily visible thickening of the right patellar ligament and mixed signals, which increased with tibial tuberosity. There were also mixed signals of adjacent soft tissues. There was also proximal tibiofibular bone fusion, and hyperosteogeny at the edges of several bones. The cartilage beneath the articular surface was smooth.
Some effusion was found in the joint cavity and joint capsule. A strip-like hyper signal was seen in the meniscus, especially in the posterior corner of the medial meniscus, with swelling of the subcutaneous soft tissue (Figure 3).
Treatment
After completing all preoperative examinations, during the operation, results showed that the patient had structural changes of the knee joint. There was uneven articular cartilage of the distal femur and proximal tibia, and osteophytes of 0.5 cm × 0.6 cm in size were visible on the lateral malleolus of bone and femur. The end of the tibial knee joint was severely deformed, and internal and lateral osteophytes had formed at the head of the joint. The anterior cruciate ligament and posterior cruciate ligament were inelastic and hard, and they were yellow in colour with many white dots. The lateral collateral ligament and the medial collateral ligament combined with the tibia were hard, inelastic, and showed poor mobility. Obvious ossification was visible from the colour and shape.
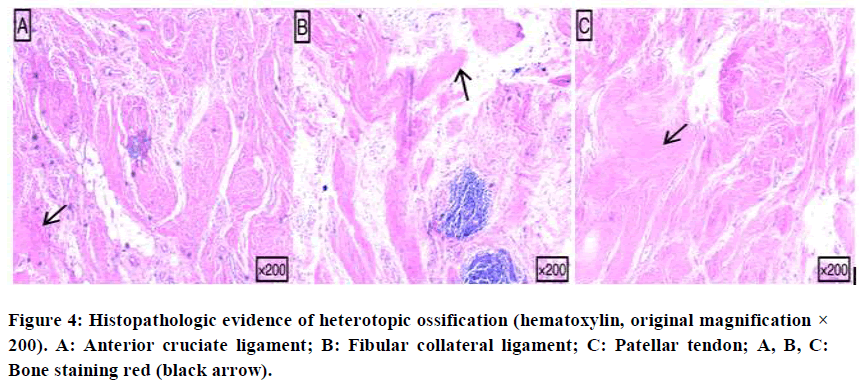
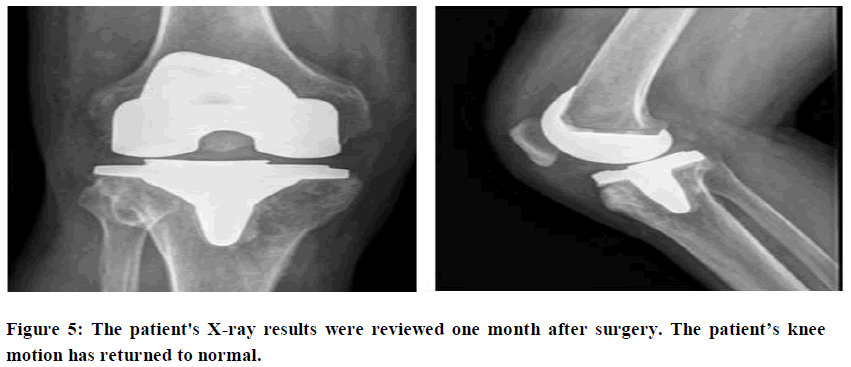
Pathologic findings showed that the patella and its ligaments were characterized by hyperplasia of fibrous and adipose tissues with infiltration of bone tissue and lymphocytes (Figure 4). The patient underwent right knee joint replacement surgery according to the preoperative plan (Figure 5). Mild leucocytosis was observed in the patient after surgery, and it was considered that this had been caused by postoperative stress. Biochemical and hematologic results were within the normal range.
We invited the patient to the hospital for review a month later surgery, and the results showed that: The postoperative knee range of motion was 0º~110º, and the VAS score was 4. The patient healed well after surgery and without adverse results.
Results and Discussion
Here, the lesion invaded the ligament around the patella, while several studies reported the ossification of the anterior cruciate ligament of the patella alone, and the lesion did not invade other surrounding tissues [9,10]. In the mentioned in their report that ossification on the meniscus may be related to joint effusion, but the specific substances that cause heterotopic ossification in joint effusion have not yet been officially identified [11]. Particularly, patients with prior issues of mental health and those requiring surgery are at even greater risk of long term mental health concerns [12].
Meniscal ossicle is relatively common in heterotopic ossification. In terms of its treatment, reported that patients with meniscal ossicles had good results with conservative treatment. In our case, the patient had severe pain during movement and severe limitation of knee movement, so surgery was the only option, leaving no room for conservative treatment [13]. Currently, many professionals believe that the best treatment for heterotopic ossification is orthopedic surgery [14,15].
Eileen MS’s (FOP) study showed that mutation of (BMP1) receptor (ACVR1) could lead to the formation of FOP due to the misregulation of BMP signal transmission and BMP resulted in heterotopic ossification by affecting the migration, differentiation, and proliferation of MSC [16]. Targeted therapy may help prevent the formation of heterotopic ossification by improving BMP signalling, but further research is needed.
Stannard classified ectopic ossification of the knee into different grades from 0 to 4 according to the severity of the disease. Among these, grade 1 and grade 2 ectopic ossifications do not involve obvious pain and do not affect joint activity, and they are not easy to detect early. Patients with grade 3 and 4 ectopic ossifications have obvious pain, and the condition interferes with joint activity, so they are readily detected by clinical examination.
In Balboni’s report, early heterotopic ossification was shown to be treatable with radiation and non-steroidal anti-inflammatory drugs [17]. It is possible that radiation and nonsteroidal anti-inflammatory drugs may prevent progression of grade 1 and 2 ectopic ossifications, but for ectopic ossification that severely affects joint mobility, only surgical treatment can improve symptoms.
Psycological distress due to osteoporosis
The behavioural changes during mental stress lead to altered dietary pattern, physical inactivity, and also threaten skeletal system. Psychological stress may be partly responsible for epigenetic regulation of skeletal development. Psychological stress is also should be recognized as a risk factor of osteoporosis [18-22].
Conclusion
Most patients facing issue such as workers compensation undergo psychological pain including reflex sympathetic dystrophy and complicated psychiatric issues. Previous research has shown that patients with better psychiatric status tend to recover quicker. Heterotopic ossification due to injury of the key ligaments around the knee requires early management. Otherwise, the lesion can quickly affect the range of motion and lead to a series of adverse outcomes. Our study shows that early diagnosis of heterotopic ossification may help prevent its progression.
Declarations
Ethics approval and consent to participate
Our institution does not require ethical approval for case report.
Consent to publish
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Availability of data and materials
The data used in this paper are from the examination department of our hospital.
Author’s contributions
AA and JLY prepared and revised the manuscript. YJJ, SWC, YP and XW performed the data collection and analysis with AA. AA, YW and JLY provides pathology assistance and picture editing work. SW and YW designed and supervised the overall study and revised the manuscript. All the authors have read and approved the manuscript.
Conflict of interests
The authors declare that they have no Conflict of interests.
Funding
Guangdong Medical Research Foundation (A2021321); The Key Discipline Building Capacity Improvement Project of Shenzhen Municipal Health Commission (201506029).
Acknowledgements
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
References
- Shehab D, Abdelhamid H, Elgazzar B, David Collier. Heterotopic Ossification. Journal of Nuclear Medicine. 2002; 43(3): 346-353.
[Google Scholar] [PubMed]
- Forsberg JA, Pepek JM, Wagner S, Wilson K, Flint J, Andersen RC, et al. Heterotopic ossification in high-energy wartime extremity injuries: prevalence and risk factors. The Journal of Bone & Joint Surgery. 2009; 91(5): 1084-1091.
[Crossref] [Google Scholar] [PubMed]
- Bossche LV, Vanderstraeten G. Heterotopic ossification: A review. Journal of Rehabilitation Medicine. 2005; 37(3): 129-136.
[Crossref] [Google Scholar] [PubMed]
- Nauth A, Giles E, Potter BK, Nesti LJ, Frederick PO, Bosse MJ, et al. Heterotopic ossification in orthopedic trauma. Journal of Orthopaedic Trauma. 2012; 26(12): 684-688.
[Crossref] [Google Scholar] [PubMed]
- Maender C, Sahajpal D, Wright TW. Treatment of heterotopic ossification of the elbow following burn injury: recommendations for surgical excision and perioperative prophylaxis using radiation therapy. Journal of Shoulder and Elbow Surgery. 2010; 19(8): 1269-1275.
[Crossref] [Google Scholar] [PubMed]
- Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. The American Journal of Sports Medicine. 2012; 40(4): 854-863.
[Crossref] [Google Scholar] [PubMed]
- Coons D, Godleski M. Range of motion exercises in the setting of burn-associated heterotopic ossification at the elbow: Case series and discussion. Burns. 2013; 39(4): e34-38.
[Crossref] [Google Scholar] [PubMed]
- Perry S, Tepperman, Hilbert L, Peters W, Pritzker K. Heterotopic Ossification in Burns. Journal of Burn Care Rehabilitation. 1984: 5(4): 283-287.
[Crossref]
- Devgan A, Mukhopadhyay R, Singh A, Gogna P, Singla R, Magu NK. Ossicle in anterior cruciate ligament: a rare occurrence. Case Reports in Orthopedics. 2014; 2014(1): 616715.
[Crossref] [Google Scholar] [PubMed]
- Sarsilmaz A, Gelal F. A new variation: An anterior cruciate ligament attached to the accessory ossicle. Clinical Anatomy. 2011; 24(8): 991-993.
[Crossref] [Google Scholar] [PubMed]
- Yu JS, Resnick D. Meniscal ossicle: MR imaging appearance in three patients. Skeletal Radiology. 1994; 23(8): 637-639.
[Crossref] [Google Scholar] [PubMed]
- Bernsetin RM, Olsson HE, Spitzer RM, Robinson KE, Korn MW. Ossicle of the meniscus. American Journal of Roentgenology. 1976; 127(5): 785-788.
[Crossref] [Google Scholar] [PubMed]
- Glass RS, Barnes WM, Kells DU, Thomas S, Campbell C. Ossicles of knee menisci. Report of seven cases. Clinical Orthopaedics and Related Research. 1975; 111(9): 163-171.
[Crossref] [Google Scholar] [PubMed]
- Stannard JP, Wilson TC, Sheils TM, McGwin G, Volgas DA, Alonso JE. Heterotopic ossification is associated with knee dislocation. Arthroscopy. 2002; 18(8): 835-839.
[Crossref] [Google Scholar] [PubMed]
- Nauth A, Giles E, Potter BK, Nesti LJ, brien FPO, Bosse MJ, et al. Heterotopic ossification in orthopedic trauma. Journal of Orthopaedic Trauma. 2012; 26(12): 684-688.
[Crossref] [Google Scholar] [PubMed]
- Shore EM, Xu M, Feldman GJ, Fenstermacher DA, Cho TJ, Choi IH, et al. A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nature Genetics. 2006; 38(5): 525-527.
[Crossref] [Google Scholar] [PubMed]
- Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: Pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. International Journal of Radiation Oncology Biology Physics. 2006; 65(5): 1289-1299.
[Crossref] [Google Scholar] [PubMed]
- Iida K, Hashimoto Y, Okazaki S, Nishida Y, Nakamura H. Surgical excision of heterotopic ossification associated with anti-N-methyl-d-aspartate receptor encephalitis: A case report. International Journal of Surgery Case Reports. 2021; 89(1):106643.
[Crossref] [Google Scholar] [PubMed]
- Hudson SJ, Brett SJ. Heterotopic ossification–a long-term consequence of prolonged immobility. Critical Care. 2006; 10(6):1-2.
[Crossref] [Google Scholar] [PubMed]
- Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. The American Journal of Sports Medicine. 2002; 30(3):447-456.
[Crossref] [Google Scholar] [PubMed]
- Sheinbein S. Psychological effect of injury on the athlete: A recommendation for psychological intervention. AMAA Journal. 2016; 29(3):8-11.
[Google Scholar]
- Mingo-Robinet J, Castañeda-Cabrero C, Alvarez V, Alonso-Cortés JM, Monge-Casares E. Tourniquet-related iatrogenic femoral nerve palsy after knee surgery: case report and review of the literature. Case Reports in Orthopedics, 2013; 2013(1):1-4.
[Crossref] [Google Scholar] [PubMed]