Introduction
Alcohol dependence is a chronic relapsing pathology, the relapse rate is relatively high, ranging from 60% to 90%. A number of studies around the world found that most alcohol-dependent patients relapsed within three to six months after being discharge from hospital, with the risk of relapse being highest in the first two months. The relapse of alcohol dependence is likely to result from a combination of various factors. Parameters involved in relapse include biological, psychological, social and spiritual factors. Some studies show that psychiatric co-morbidity, alcohol dependence severity, craving, use of other substances, health and social factors are consistently significantly associated with alcohol dependence relapse [1]. Conversely, supportive social network factors, self-efficacy, and factors related to purpose and meaning in life, are protective against alcohol dependence relapse [2].
The sociological demographic characteristics are considered to be one of the factors associated to the alcohol dependence relapse. The alcohol-dependent patients that are single are more likely to relapse than those who are married. Relapse also tends to be more serious to the unemployed group. The risk of serious alcohol problems is 3-4 times higher in the family members of those with alcohol use disorders, the rate increases with the larger number of family members, more serious alcohol disorders, closer genetic relationships. Besides, cutural traditions, customs and ethics are also important factors associated with the level of alcohol abuse as well as promoting the relapse after alcohol detoxification of each individual in each region. Many Western societies have a open minded attitude towards alcohol drinking. In Vietnam, that men drink alcohol is considered normal, reflecting masculine power, meanwhile women who drink alcohol are often severely criticized, so the subject that abuse and was depended on alcohol was mainly male [3].
A number of alcohol use characteristics considered to be associated with the relapse are cravings, group pressure, age at first using alcohol, duration of alcohol use, times of alcohol withdrawal as well as preventive treatment for alcohol dependence relapse. The studies of Bottlender and Soyka, Evren et al. Korlakunta et al. Kuria all found that strong cravings for alcohol is one of the factors associated with the alcohol dependence relapse. The study of Jin et al. also found no difference in the age at first using alcohol and the duration of alcohol use of the relapse and the non-relapse groups [4].
An important factor also related to alcohol dependence has been mentioned by many researchers, which is the co-occuring between alcohol dependence and some mental disorders. Approximately 30%-40% of alcohol-dependent patients meet the diagnosis criteria of depressive disorder at a certain time throughout their lives and vice versa. 25%-50% of those with alcohol-related disorders meet the diagnostic criteria of an anxiety disorder, especially phobias and panic disorders. This research aims to analyze some factors associated with the alcohol dependence relapse in the alcohol-dependent patients who have been detoxified in northern Vietnam [5].
Material and Methods
Study design
This is a prospective study. The alcohol-dependent patients were monitored during the time admitted to national institute of mental health-Bach Mai hospital and at the points of one month, three months and six months after being discharged from the hospital to the community in northern Vietnam [6].
Study settings: Bach Mai hospital in Hanoi is the key hospital in northern Vietnam which is equipped with 3200 beds with 56 affiliated units, including 4 institutes, 14 centres, 9 functional departments, 27 clinical departments and Bach Mai medical college, journal of clinical medicine and service unit. The national institute of mental health belongs to Bach Mai hospital. The institute consists of eight clinical departments (out-patient, stress-related disorder, child psychiatry, schizophrenic disorder, mood disorder, substance abuse, psychogeriatric and clinical psychology) with 257 inpatient beds. On average, the institute examines and treats 250-280 inpatients and 300-350 out-patients per day.
Inclusion criteria: We selected the patients who were admitted to the national institute of mental health-Bach Mai hospital having alcohol dependence according to the International Classification of Diseases, the 10th edition (ICD-10).
Exclusion criteria: Excluded from the study were the participants suffering from severe medical problems.
Participants
122 Vietnamese patients with mental and behavioral disorders caused by alcohol use who met the criteria for the diagnosis of alcohol dependence according to ICD-10, were admitted to national institute of mental health-Bach Mai hospital in 2018-2019 and agreed to participate in the study. All the patients live in northern Vietnam. The reasons for hospitalization were the symptoms of withdrawal syndrome or alcohol psychosis or sleeplessness, etc. A total of 122 patients were observed for a period of six months, 21 patients dropped out due to various reasons including not wanting to continue to participate in the study, inconvenience due to long distance from home to the hospital, etc [7].
Measures
Variables used: Background characteristics of study participants were: Age, gender, educational background, occupation and marital status [8].
Variables related to alcohol dependence and relapse consisted of the sociological demographic characteristics of the research group, alcohol consumption (number of standard drinks), type of alcohol use, the common drinking place, relapse of alcohol dependence, time of relapse after discharge, the reasons for relapse, time of alcohol withdrawal, the adherence to treatment and co-occurring mental disorders [9].
Study tools: A standard drink was defined as containing 10 g of pure alcohol (equivalent to 12.5 ml of pure alcohol). A standard drink was equivalent to 285 ml full-strength beer (4.8% alcohol), 425 ml low strength beer (2.7% alcohol), 275 pre-mix spirits (5% alcohol), 100 ml wine (13.5% alcohol), 30 ml spirits (40% alcohol) (International Center for Alcohol Policies (ICAP), Geneva, World Health Organisation).
Relapse of alcohol dependence was defined as the patient met the criteria for the diagnosis of alcohol dependence according to ICD-10 after a period of abstinence [10].
Alcohol dependence, relapse and co-occurring mental disorders with alcohol dependence were diagnosed by clinical psychiatrists, using the International Classification of Diseases, the 10th edition (ICD-10). Depression was defined using the Hamilton Depression Rating Scale (HDRS). The total score ranges from 0 to 52. Score 0-7: no depression. Score 8-13: mild depression. Score 14-18: moderate depression. Score 19-22: severe depression. Score over 23: very severe depression. Anxiety was defined using the Hamilton Anxiety Rating Scale (HARS). HARS consists of 14 questions. The points present five corresponding levels from ‘none’ to ‘very severe’: 0. none; 1. mild; 2. moderate; 3. severe; 4. very severe. The total score under 14: no anxiety; score 14-17: mild anxiety; score 18-24: moderate anxiety; score 25-30: severe anxiety, score over 30: very severe anxiety. These psychological tests were verified by Cronbach's alpha with good and acceptable reliability. The reliability of the HDRS was 0.879. The reliability of the HARS was 0.897 [11].
Data collection: During the time admitted at the hospital, the patients were interviewed to gather information about alcohol use and related situation. The patients were assessed via a comprehensive clinical examination to get the final diagnosis of alcohol dependence and co-occurring psychiatric disorders by qualified psychiatrists, using ICD-10. The selected patients were then performed psychological tests to detect depression using Hamilton depression rating scale, accompanying anxiety using Hamilton anxiety rating scale when they cooperated. During hospitalized detoxification, all participants received pharmacological therapies for symptomatic and supportive treatment which were up to the physicians, the researchers did not interfere with the treatment process. All participants were given general health education to encourage them to remain abstinence or come to further clinical assessment for their relapse at the follow-up interviews. At the point of one month, three months and six months after being discharged from hospital, the patients were monitored alcohol consumption, relapse of alcohol dependence, co-occurring psychiatric disorders using ICD-10, Hamilton depression rating scale, Hamilton anxiety rating scale in the hospital or in their home. The total data collection process was done by qualified psychiatrists and psychologists [12].
Statistical analysis
Data analyses were performed using Stata 15 software. Descriptive statistics included the estimates of the frequency and the proportion of qualitative variables. Mean values were used to describe quantitative variables. Poisson regression model analyzed relapse rate during follow-up: Dependent variable (number of relapse during follow-up time based on assessment time), independent variable (demographic characteristic, alcohol use characteristics and co-occurring psychiatric disorders), producing adjusted odds ratios and 95% of the confidence intervals [13].
Results
General characteristics of the study participants
Of the 101 participants in the study, the majority of alcohol-dependent patients was male (99.01%), mainly employed 97.03%. Within which, the group of patients with secondary school education accounted for the highest proportion (38.61%). 83.17% of the patients were married. The average age of study subjects was: 47.85 ± 9.31. The average age at first use of alcohol was 20.62 ± 5.60 (Table 1).
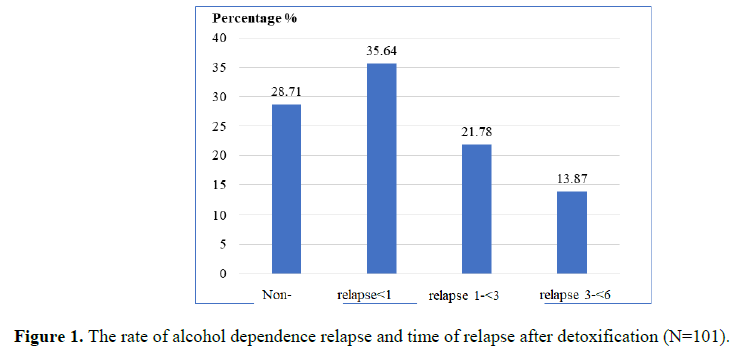
The rate of alcohol dependence relapse and time of relapse after detoxification
The rate of alcohol dependence relapse was 71.29%. The rate of relapse was highest in the first month after detoxification (35.64%), then gradually decreased over time (Figure 1) [14].
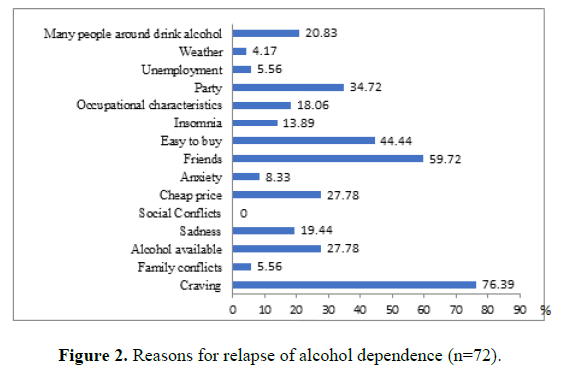
Reasons for alcohol dependence relapse
There were many reasons that the subjects relapsed into alcohol dependence, accounting for the largest proportion of their cravings: 76.39% (Figure 2).
Poisson regression model for relapse during follow up demographic characteristics, alcohol use characteristics and co-occurring psychiatric disorder
Poisson regression model explains 13.39% of the variation in the rate of dependence relapse in the research group. Patients with education from high school and higher had relapse rate of 0.65 times as compared to patients with education below high school (IRR=0.65; 95% CI: 0.43-0.99). Patients with four or more times of alcohol withdrawal had a relapse rate of 1.76 times compared with patients with less than 4 times of alcohol withdrawal (IRR=1.76; 95% CI: 1.09-2.84). Patients with moderately depressive disorder on the Hamilton depression rating scale at the time admitted at the hospital had a relapse rate of only 0.44 times that of patients without depression (IRR=0.44; 95% CI: 0.2-0.97). Patients with severe and very severe depressive disorders on the Hamilton depression rating scale at 1 month after being discharge from hospital had a relapse rate of 4.27 times that of non-depressed patients. (IRR=4.27; 95% CI: 1.08-16.97) (Table 2) [15].
| Characteristics |
n |
(%) |
| Gender |
Male |
100 |
99.01 |
| Female |
1 |
0.99 |
| Occupation |
Employed |
98 |
97.03 |
| Unemployed |
3 |
2.97 |
| Academic level |
Primary school |
7 |
6.93 |
| Secondary school |
39 |
38.61 |
| High school |
37 |
36.63 |
| College, university, postgraduate |
18 |
17.83 |
| Marital status |
Married |
84 |
83.17 |
| Single, separated/divorced |
17 |
16.83 |
| The average age |
47.85 ± 9.31 |
| The average age for the first time using alcohol |
20.62 ± 5.60 |
Table 1. General characteristics of the study participants.
| Variables (reference group) |
Incidence Rate (IRR) |
p |
95% CI |
| Age of patient (<40 years) |
Age ≥ 40 |
0.74 |
0.287 |
0.42 |
1.29 |
| Marital status (Marriage) |
Single/divorced/widowed |
1.08 |
0.764 |
0.64 |
1.83 |
| Educational attainment (below high school) |
≥ High school |
0.65 |
0.043 |
0.43 |
0.99 |
| Age of initiation of alcohol use (<30 years old) |
From 30 years old |
0.68 |
0.236 |
0.36 |
1.29 |
| Alcoholism period (<20 years) |
From 20 years |
0.8 |
0.313 |
0.52 |
1.23 |
| Number of detoxification attempts (<4 times) |
≥ 4 times |
1.76 |
0.02 |
1.09 |
2.84 |
| Compliance of treatment (No) |
Adhere to 3 times |
0.69 |
0.069 |
0.46 |
1.03 |
| Depressive disorder at the time admitted at the hospital (No) |
Mild |
0.93 |
0.798 |
0.54 |
1.62 |
| Moderate |
0.44 |
0.042 |
0.2 |
0.97 |
| Serious, very serious |
0.45 |
0.057 |
0.2 |
1.03 |
| Depressive disorder at 1 month (No) |
Mild |
1.53 |
0.277 |
0.71 |
3.28 |
| Moderate |
1.21 |
0.743 |
0.38 |
3.86 |
| Serious, very serious |
4.27 |
0.039 |
1.08 |
16.97 |
| Depressive disorder at 3 months (No) |
Mild |
0.77 |
0.329 |
0.45 |
1.31 |
| Moderate |
0.81 |
0.741 |
0.24 |
2.74 |
| Serious, very serious |
2.26 |
0.245 |
0.57 |
8.9 |
| Depressive disorder at 6 months (No) |
Mild |
1.23 |
0.621 |
0.54 |
2.79 |
| Moderate |
0.35 |
0.236 |
0.06 |
1.97 |
| Serious, very serious |
- |
- |
- |
- |
| Anxiety disorder during hospitalization (No) |
Mild |
1.69 |
0.243 |
0.7 |
4.08 |
| Moderate |
0.97 |
0.927 |
0.51 |
1.85 |
| Serious, very serious |
1.35 |
0.5 |
0.56 |
3.24 |
| Anxiety disorder at 1 month (No) |
Mild |
1.16 |
0.784 |
0.4 |
3.35 |
| Moderate |
0.66 |
0.487 |
0.2 |
2.13 |
| Serious, very serious |
0.4 |
0.473 |
0.03 |
4.93 |
| Anxiety disorder at 3 months (No) |
Mild |
0.85 |
0.706 |
0.37 |
1.96 |
| Moderate |
1.04 |
0.959 |
0.23 |
4.75 |
| Serious, very serious |
0.99 |
0.992 |
0.16 |
6.03 |
| Anxiety disorder at 6 months (No) |
Mild |
0.99 |
0.984 |
0.51 |
1.93 |
| Moderate |
0.96 |
0.936 |
0.35 |
2.6 |
| Serious, very serious |
0.44 |
0.351 |
0.08 |
2.44 |
| Group pressure at 1 month (No) |
Yes |
1.41 |
0.323 |
0.72 |
2.76 |
| Group pressure at 3 months (No) |
Yes |
1.87 |
0.279 |
0.6 |
5.78 |
| Group pressure at 6 months (No) |
Yes |
0.42 |
0.128 |
0.13 |
1.29 |
| Psychological trauma at 1 month (No) |
Yes |
0.69 |
0.311 |
0.34 |
1.41 |
| Psychological trauma at 3 months (No) |
Yes |
0.44 |
0.255 |
0.11 |
1.81 |
| Psychological trauma at 6 months (No) |
Yes |
3.16 |
0.077 |
0.88 |
11.32 |
| Coefficient of incidence at the beginning |
2.74 |
0.023 |
1.15 |
6.54 |
Note: Pseudo R2=0.1339; Pearson goodness of fit: 69.20652; Prob>chi2(63)=0.276
Table 2. Poisson regression model of relapse during follow-up on demographic characteristics, alcohol use characteristics and co-occurring psychiatric disorder (N=101).
Discussion
Alcohol dependence relapse
As reported by Nguyen and Nguyen, Thompson and colleagues, the rate of relapse was 60% to 90% despite the treatment intervention. Walitzer and Dearing’s research also found this rate to be around 70%. According to our study, 71.29% of patients had a relapse after the cessation. The rate of relapse was relatively high in general. The highest relapse rate was in the first month after alcohol cessation, accounting for about 35.64%. The rate then gradually decreased with time milestones. These findings were consistent with the research of Neto and colleagues. This implies the need for positive treatment measures to prevent relapse for alcohol-dependent patients immediately after detoxification.
Reasons for relapse of alcohol dependence
There were many reasons for relapse of alcohol dependence, of which the largest proportion was due to cravings (76.39%). Some researchers in the world also made the same comment as us. According to Zywwiak et al. cravings were the most important cause of relapse. Bottlender va Soyka also identified strong alcohol cravings as one of the prognostic factors for alcohol relapse.
This can be explained by changes in brain biochemistry in chronic alcoholics who lack alcohol for a long time, creating an imbalance in the nervous system, leading to post-drinkers. When quitting, it was easy to have the urge to use alcohol again. For this reason, after detoxification, alcohol-dependent patients need counseling and guidance to recognize the craving for alcohol as a warning sign of alcohol reuse and relapse behavior. Thereby helping them develop coping skills to prevent relapse.
Poisson regression model for relapse during tracking demographic characteristics, alcohol use characteristics and occurring psychiatric disorder
Poisson's regression results strongly reinforce that alcohol-dependent patients had many previous alcohol withdrawal times, the co-occurrence of depressive disorder increased alcohol dependence relapse and relapsed soon after recovering from alcohol dependence. In particular, higher education was a protective factor against relapse, possibly due to a better awareness of the harmful effects of alcohol. Several studies from many European countries proved that adolescents with lower academic level frequently had health risk behaviours, especially alcohol use. Therefore, it was more difficult for this group to maintain the non- alcohol use period after cessation in Vietnam as well as in other countries.
Some studies in the world showed the connection between marital status and age of patients with alcohol dependence relapse. According to Walitzer and Dearing, a single alcohol-dependent patients were more likely to relapse than a married one. Marriage was considered as a protective factor, especially in males. The study of Walter et al., also found that a single alcohol-dependent patient was twice as likely to relapse than a married one. Some studies such as that of Jakubczyk et al, Spruyt et al, Evren et al found no association between age and relapse into alcohol dependence. After examining some of the factors associated with the alcohol dependence relapse in this group, we found that there was no connection between marital status and the age of a patient with alcohol dependence relapse, p>0.05. The differences among the studies may result from the size of samples and the inadequate observing period.
There was no connection between age at first drink, duration of alcohol consumption with the alcohol dependence relapse. As reported in the study of Jin et al, there was no difference in the age at first drink and the duration of alcohol consumption between the relapse group and the non-relapse group, which was the same as our study results. However, evidence showed that about 90% of alcohol-dependent patients were likely to relapse at least once in about four years after treatment. Alcohol dependence patients who have had multiple alcohol withdrawal and relapse attempts have demonstrated the difficult nature of quitting alcohol and may be due to inadequate access to effective anti-relapse treatment. Around the world, there were many studies investigating the relationship between mental disorders and alcohol dependence relapse. The study of Korlakunta et al., Driessen et al., which observed that depression increased the risk of alcohol dependence. These findings were consistent with our study. Therefore, the early detection and treatment of simultaneous psychiatric disorders in alcohol-dependent patients will contribute to reducing the risk of relapse. However, our study found no association between anxiety disorders and psychological trauma with relapse. According to Schellekens et al., anxiety disorder prognoses early relapse and the study of Trocchio et al., also noted this association. In addition, there was a significant association between sleep disturbance and alcohol dependence relapse and sleep disorders increased the risk of relapse. Research by Evren et al., Sureshkumar et al. confirmed that many past stressful events were associated with relapse. With a larger sample size and a longer study period, the association between co-occurring psychiatric disorders and alcohol dependence relapse will be more conspicuous and more similar to other studies around the world.
Conclusion
The rate of relapse among alcohol-dependent inpatients in Northern Vietnam remains at a high level. They relapsed rapidly after their discharge from the hospital with many reasons, especially craving. Number of withdrawal times and depression were the risk factors for alcohol dependence relapse. In particular, higher education was a protective factor against relapse. These factors were depended on economic, medical, cultural and social characteristics in different countries. Thus, alcohol dependence is a not only pathological but also social problem, the coordination of many departments as well as the families and the patients’ determination is needed in order to find solutions to reduce the relapse rate.
Ethical Considerations
Patients were clearly explained the objectives and methods of the study, signed a consent form to participate in the study and had the right to withdraw from the study without explanation. They were informed that no discrimination in treatment would happen if they declined to participate in the study at any time. The patients’ information was coded and kept confidential. The study was approved by the ethics committee-Hanoi medical university (decision number 09NCS17/HMU IRB).
Acknowledgements
We would like to thank the participants and their family members in this study, as well as the staff of Vietnam national institute of mental health-Bach Mai hospital for supporting us in implementing this study.
Funding
We received no funding for this work.
Availability of Data and Materials
The dataset generated during the current study is not publicly available due to the protection of personal data within the study but is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the ethics committee
of Hanoi medical university (decision number
09NCS17/HMU IRB). A written consent form
was signed and given by all participants.
Competing Interests
We report no conflict of interest concerning this
study.
References
- Albert PR. Why is depression more prevalent in women. J Psych Neurosci. 2015;40(4):219-221.
[Crossref] [Google Scholar] [PubMed]
- Sang WJ, Meysam, A, Yong-Ku K. Bio-psycho-social risk factors for depression. Major Depres Disord. 2017;71-90.
- Almanzar S, Shah N, Vithalani S, Shah S, Squires J, et al. Knowledge of and attitudes toward clinical depression among health providers in Gujarat, India. Ann Global Health. 2014;80(2):89-95.
[Crossref] [Google Scholar] [PubMed]
- Evans-Lacko SA. Socio-economic variations in the mental health treatment gap for people with anxiety, mood and substance use disorders: Results from the WHO World Mental Health (WMH) surveys. Psych Med. 2018;48(9):1560-1571.
[Crossref] [Google Scholar] [PubMed]
- Leng CS, Hutagalung FD, Li LP. A review of depression and its research studies in Malaysia. Int J Educ. 2017;2:40-55.
[Google Scholar]
- Ng CG. A review of depression research in Malaysia. Med J Malaysia. 2014;69:42-45.
[Google Scholar] [PubMed]
- Nur Saadah, MA, Noremy M. Empowering informal caregivers and care for family. Int J Academic Res Bus Soc Sci. 2021;11(3):444-452.
[Google Scholar]
- Idris A, Md Akhir N, Mohamad MS, Sarnon N. Exploring the lived experience on recovery from Major Depressive Disorder (MDD) among women survivors and five CHIME concepts: A qualitative study. Behav Sci. 2023;13(2):151.
[Crossref] [Google Scholar] [PubMed]
- Siti MZ, Nurul SS, Noremy MA, Suzana MH, Jamiah M. Single mother life challenges: Impact on emotional well-being. Int J Edu Psychol Counsel. 2019;4(24):69-84. [Google Scholar]
- Ogbo FA, Mathsyaraja S, Koti RK, Perz J, Page A. The burden of depressive disorders in South Asia, 1990-2016: Findings from the global burden of disease study. BMC Psych. 2018;18(1):1.
[Crossref] [Google Scholar]
- Bjornestad J, Ten VHW, Joa I, Davidson L, Larsen TK, et al. With a little help from my friends social predictors of clinical recovery in first-episode psychosis. Psych Res. 2017;255:209-214.
[Crossref] [Google Scholar] [PubMed]
- Bjorlykhaug KI, Karlsson B, Hesook SK, Kleppe LC. Social support and recovery from mental health problems: A scoping review. Nordic Soc Work Res. 2022;12(5):666-697.
[Crossref] [Google Scholar]
- Jacob KS. Recovery model of mental illness: A complementary approach to psychiatric care. Indian J Psychol Med. 2015;37(2):117-119.
[Crossref] [Google Scholar] [PubMed]
- Kader MSF, Mohd SS, Rampal L, Mukhtar F. Prevalence associated factors and predictors of depression among adults in the community of Selangor, Malaysia. PloS One. 2014;9(4):e95395.
[Crossref] [Google Scholar] [PubMed]
- Kovacs M, Obrosky S, George C. The course of major depressive disorder from childhood to young adulthood: Recovery and recurrence in a longitudinal observational study. J Affect Disord. 2016;203:374-381.
[Crossref] [Google Scholar] [PubMed]
Citation: Alcohol-Dependent Inpatients in Northern Vietnam: A Prospective Study on Factors Related to Relapse. ASEAN Journal
of Psychiatry, Vol. 24 (7) September, 2023; 1-8.